Ankylosing Spondylitis (Bechterew’s disease) – A Pain in the Back
They say that college is the best years of your life. Looking back on it, there were many things I did and experienced in college. But back pain was not one of them. I know what you’re asking: “Why would you have back pains in your 20’s and 30’s?. Did you experience some kind of trauma? Do you have scoliosis?” No!
I always thought something was not right. But when I sought professional help, I would always be told, “You’re too young for back pain!”


I had always known I had bad posture from years of being a lifeguard and hunching over a desk. But this was different. As the years progressed after college, the pain in my lower back got worse. I would “throw out” my back approximately every 6 months. Then, every two to three months. Then it was every morning, making sure to do stretches to ensure any repeated bouts of pain wouldn’t occur.
The pain would be intense in the morning and go away by the afternoon – sometimes by night. The process would repeat daily. I was prescribed almost every type of muscle relaxer on the market. The pain specialist whom I was seeing at the time referred me to a physical therapist and suggest acupuncture and message therapy. Physical therapy helped with correcting the posture and gave a little relief. Acupuncture and massages helped me relax in the moment. But sure enough, the next day, I was right back where I started. At my final breaking point, the doctor referred me to a rheumatologist. It was here that I was diagnosed with Ankylosing Spondylitis.
Ankylosing spondylitis (Bechterew’s Disease), or “AS” for short, is not commonly known unless you have it. No – it’s not a special character in a video game or a type of fungus you should avoid. Ankylosing Spondylitis is a form of arthritis that mainly affects the spine and sacroiliac joints (lower back). An inflammatory disease, symptoms of Ankylosing Spondylitis include pain, stiffness, and in some cases, loss of mobility. AS is often difficult to diagnose. And in some instances, misdiagnosed initially.
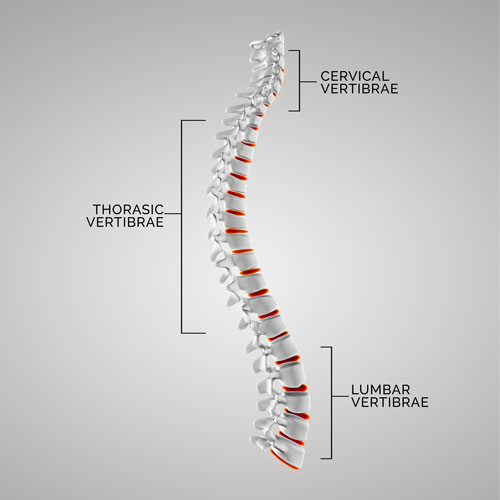
Pain is the main symptom, especially in the lower back and buttock areas. Inflammation and pain are not confined to the spine, however. It can affect other parts of the body such as the neck, shoulder, knees, ribcage, feet (often in the arch and heel of the foot). If left untreated it can cause inflammation to spread to the organs, such as your bowels, lungs, and/or heart. The disease involves erosion of bone and increased bone formation in the spine, leading to bone fusion. In advanced cases, this can lead to spinal deformity.
The joints that are first affected are typically the sacroiliac (SI) joints. A common sign of AS is pain in the morning – after sleep or long durations of inactivity – that gradually recedes as the day progresses, or when exercise is introduced. Staying active is difficult—but it’s essential. Exercise, even in small amounts, can help maintain flexibility and posture. Individuals have found that swimming, walking, cycling, light strength training, Tai Chi, Yoga, Pilates, and overall stretching can help manage AS symptoms.

Diagnosing AS is often tricky and leads to misdiagnoses and sometimes no diagnosis at all. Typically, a rheumatologist would be the physician who would diagnose AS. A thorough physical exam may help diagnosis AS, and include X-rays, individual medical history, blood work (including tests for HLA-B27), and a research on family history of AS.
The joints that are first affected are typically the sacroiliac (SI) joints. A common sign of AS is pain in the morning – after sleep or long durations of inactivity – that gradually recedes as the day progresses, or when exercise is introduced. Staying active is difficult—but it’s essential. Exercise, even in small amounts, can help maintain flexibility and posture. Individuals have found that swimming, walking, cycling, light strength training, Tai Chi, Yoga, Pilates, and overall stretching can help manage AS symptoms.
Once diagnosed, common treatment may consist of exercise, physical therapy, and medications. Medication can include Non-steroidal anti-inflammatory drugs (NSAIDs) which can relieve inflammation, pain, and stiffness. If NSAIDs aren’t helpful, your doctor might suggest starting a biologic medication, such as a tumor necrosis factor (TNF) blocker, or an interleukin 17 (IL-17) inhibitor. TNF blockers target a cell protein that causes inflammation in the body. TNF blockers help reduce pain, stiffness, and tender or swollen joints. They are administered by injecting the medication under the skin or through an intravenous line. For advanced cases of AS, surgery is sometimes needed.
The five TNF blockers approved by the Food and Drug Administration to treat Ankylosing Spondylitis are:






Secukinumab (Cosentyx) is the first IL-17 inhibitor approved by the FDA for the treatment of ankylosing spondylitis.
“The combination of medications and staying active are great first steps, but paying attention to what you put in your body is equally important.”
– GG, RE Pharmacy Contributing Author
Keeping a healthy diet is often a struggle for many people. Easy access to fast food, junk foods and microwave-ready foods are often used in lieu of healthier options. Eating plenty of fruits and vegetables, including colorful antioxidants and mineral-rich options, will keep you on the right path. Calcium and Vitamin D are crucial in preventing osteoporosis, which is a common and high risk for individuals with AS. One way to do this is having an anti-inflammatory diet in which you replace sugars and refined foods with whole, nutrient-rich foods.
Ankylosing Spondylitis treatment is complex and has many variables, but so is the human body as a whole. There is no cure for AS. But open communication with your doctor, along with a set treatment plan (medications, diet, and lifestyle changes), you can slow down and manage the progression of the disease.

To read more on Ankylosing Spondylitis, please visit:
https://www.mayoclinic.org/diseases-conditions/ankylosing-spondylitis/symptoms-causes/syc-20354808

Jennifer “Lizzie” MacDonald leads the PATH – Patient Healthcare and Wellness Program at River’s Edge Pharmacy. As a patient with multiple chronic conditions, Lizzie has first-hand experience with navigating the complex health system.
Throughout her journey, she has become impassioned with sharing her knowledge and serving as an ambassador for patient independence, wellness, and recovery. This not only lead to patients’ relief and comfort, it has provided an opportunity for doctors to utilize a patient advocate for more effective and time-saving care in their practices.
Lizzie is an outspoken supporter of creating community through support groups as well as through the invaluable connection of one-on-one interactions for patients who are managing chronic/complex illnesses. Through her efforts, she has emboldened patients to share their ideas, goals, and triumphs, as well as live life to the fullest, regardless of their condition(s).
Lizzie is also a contributing author to River’s Edge Pharmacy’s News and Articles









